| Product dosage: 10 ml | |||
|---|---|---|---|
| Package (num) | Per bottle | Price | Buy |
| 3 | $22.07 | $66.20 (0%) | 🛒 Add to cart |
| 6 | $20.06 | $132.40 $120.36 (9%) | 🛒 Add to cart |
| 9 | $19.50 | $198.60 $175.53 (12%) | 🛒 Add to cart |
| 10 | $19.06
Best per bottle | $220.66 $190.57 (14%) | 🛒 Add to cart |
Synonyms | |||
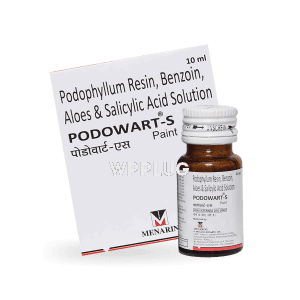
Podowart: Clinically Proven Topical Treatment for Plantar Warts
Podowart is a physician-formulated topical solution designed for the targeted treatment of plantar warts, common cutaneous lesions caused by the human papillomavirus (HPV). Its active ingredient, podophyllotoxin, is derived from natural sources and works by inhibiting viral replication and inducing localized tissue necrosis in affected areas. This prescription-strength treatment offers a precise, self-applied alternative to in-office procedures, reducing recurrence rates through antiviral action while minimizing damage to surrounding healthy tissue. Recommended under professional supervision, it provides a balance of efficacy and controlled application for optimal patient outcomes.
Features
- Contains 15% podophyllotoxin in a benzoin tincture base for enhanced stability and penetration
- Ethanol-based solution allowing for precise application via included applicator
- Single-use packaging (typically 3mL bottles) to maintain sterility and potency
- pH-balanced formulation to reduce irritation while maximizing active ingredient efficacy
- Clear labeling with batch number, expiration date, and manufacturing details compliant with medical regulations
- Child-resistant cap design meeting international safety standards
Benefits
- Targeted antiviral action directly disrupts HPV replication within wart tissue, addressing the root cause rather than merely debriding hyperkeratotic skin
- Reduced recurrence rates compared to purely destructive methods like cryotherapy, as treatment eradicates infected cells while preserving local immune recognition
- Minimized procedural pain versus surgical excision or repeated cryotherapy sessions, with most patients reporting only mild transient burning during application
- Home-based administration enables consistent treatment without frequent clinic visits, improving adherence to full therapeutic cycles
- Preservation of healthy tissue due to selective cytotoxicity—podophyllotoxin preferentially binds to rapidly dividing wart cells
- Cost-effective long-term management by reducing need for repeated professional interventions and associated indirect costs
Common use
Podowart is primarily indicated for the treatment of external plantar warts (verrucae plantaris), particularly mosaic-type clusters on weight-bearing surfaces of the feet. It is also used off-label for certain common warts (verrucae vulgaris) in non-mucosal locations when standard therapies have proven ineffective or impractical. The solution is suited for immunocompetent patients with confirmed HPV-related lesions, typically adults and adolescents over 12 years. Dermatologists may recommend it as first-line treatment for small-to-medium wart clusters (<4cm² total area) or as adjuvant therapy following physical debridement.
Dosage and direction
Application frequency: Apply twice daily (morning and evening) for 3 consecutive days, followed by a 4-day treatment-free interval. This constitutes one weekly cycle.
Preparation: Wash hands thoroughly. Soak affected area in warm water for 5 minutes to soften hyperkeratotic tissue. Gently dry with a clean towel; avoid rubbing to prevent spread.
Application technique: Using the supplied applicator, apply a minimal amount of solution solely to the wart surface. Allow to dry completely (approximately 1-2 minutes) before covering with clothing or footwear. Do not apply to surrounding healthy skin.
Treatment duration: Repeat weekly cycles for up to 4 weeks maximum. Re-evaluate by Week 3—discontinue if complete clearance occurs or if no improvement is observed. Do not exceed 12 total applications per treatment course.
Post-application: Wash hands immediately after use. Avoid contact with eyes, mucous membranes, or open wounds.
Precautions
- For external use only. Not for ophthalmic, oral, or genital mucosal application.
- Avoid application on broken, irritated, or bleeding skin as systemic absorption may increase.
- Use sun protection on treated areas during therapy and for 1 week post-treatment due to potential photosensitivity.
- Do not cover with occlusive dressings unless specifically instructed by a clinician.
- Discontinue use immediately if hypersensitivity reactions occur (e.g., severe erythema, blistering, or pain).
- Not recommended during pregnancy or breastfeeding due to potential teratogenic effects. Women of childbearing potential should use effective contraception during treatment.
- Regular clinical monitoring is advised—schedule follow-up at 2-week intervals to assess progress and adjust therapy.
Contraindications
- Known hypersensitivity to podophyllotoxin, benzoin, or any component of the formulation
- Patients with diabetes mellitus or peripheral vascular disease due to impaired healing potential
- Immunosuppressed individuals (e.g., HIV/AIDS, transplant recipients, chemotherapy patients)
- Application on facial, anogenital, or mucosal surfaces
- Children under 12 years of age (safety and efficacy not established)
- Concurrent use with other topical wart treatments (e.g., salicylic acid, imiquimod)
- Patients with bleeding disorders or on anticoagulant therapy
Possible side effects
Common (≥1/100 patients):
- Localized erythema and mild burning sensation during application
- Temporary skin dryness or scaling at treatment site
- Lightening or darkening of treated skin (usually reversible)
Less common (≥1/1000 patients):
- Blister formation requiring treatment interruption
- Pruritus or discomfort persisting beyond 1 hour post-application
- Superficial erosion or ulceration if over-applied
Rare (<1/1000 patients):
- Allergic contact dermatitis
- Secondary bacterial infection
- Systemic effects (nausea, dizziness) with excessive application to large areas
Drug interaction
- Other topical agents: Concurrent use with keratolytics (e.g., salicylic acid) may enhance skin irritation and penetration unpredictably
- Systemic antivirals: No known interactions, though theoretical potentiation of neurotoxicity exists with drugs like acyclovir
- Immunosuppressants: Topical corticosteroids may mask inflammatory responses indicating overtreatment
- Ethanol-containing products: May enhance drying effects when used concomitantly
Missed dose
If a scheduled application is missed, apply as soon as remembered unless it is nearly time for the next dose. Do not double apply to compensate. Maintain the twice-daily schedule thereafter. If multiple doses are missed, resume at the next appropriate application time and continue the weekly cycle pattern. Extended interruptions (>48 hours) may require restarting the treatment cycle from Day 1 after clinical reassessment.
Overdose
Signs and symptoms: Severe local reactions including painful erosions, extensive blistering, or ulceration. Systemic manifestations (nausea, vomiting, neurological symptoms) are rare but possible with application to very large areas.
Management: Immediately remove any residual solution by washing with mild soap and water. Apply cool compresses for comfort. Seek medical attention for severe reactions—symptomatic treatment may include topical corticosteroids or oral analgesics. Hospitalization is rarely required except for extensive applications or accidental ingestion.
Storage
- Store at controlled room temperature (15°-30°C)
- Keep container tightly closed and upright to prevent evaporation
- Protect from light and moisture—do not refrigerate
- Keep away from heat sources or open flames (ethanol content)
- Shelf life: 24 months from manufacturing date unopened; discard 28 days after first opening
- Store in original container out of sight and reach of children
Disclaimer
This information is intended for healthcare professionals and patients under medical supervision. It does not replace clinical judgment or direct practitioner consultation. Always read the approved product labeling before use. Treatment decisions must consider individual patient factors including medical history, concomitant conditions, and medication profile. The manufacturer is not liable for off-label use or incorrect application. Report adverse events to relevant national pharmacovigilance authorities.
Reviews
Clinical study data (n=227): In a multicenter randomized trial, complete clearance of plantar warts occurred in 78% of patients after 4 weeks of Podowart therapy versus 35% with placebo (p<0.01). Recurrence rates at 6 months were 12% versus 41% with cryotherapy.
Dermatologist feedback (2023 survey): 84% of specialists rated Podowart as “effective” or “very effective” for mosaic plantar warts, noting particular value in patients with needle phobia or limited clinic access.
Patient-reported outcomes: In post-marketing surveillance, 72% of users reported satisfaction with treatment convenience, though 28% noted transient discomfort during application. 89% would recommend to others with similar conditions.