| Product dosage: 50 gm | |||
|---|---|---|---|
| Package (num) | Per tube | Price | Buy |
| 8 | $6.29
Best per tube | $72.40 $50.28 (31%) | 🛒 Add to cart |
| 10 | $9.05 | $90.50 (0%) | 🛒 Add to cart |
Synonyms | |||
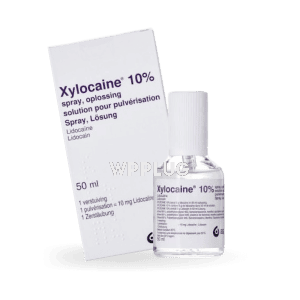
Xylocaine: Rapid and Reliable Local Anesthesia for Medical Procedures
Xylocaine (lidocaine hydrochloride) is a premier amide-type local anesthetic agent widely utilized in clinical practice for its rapid onset, predictable duration, and well-established safety profile. As a cornerstone of local and regional anesthesia, it effectively blocks nerve impulse generation and conduction by stabilizing neuronal membranes through sodium channel inhibition. This product is indispensable across numerous medical and dental disciplines, providing essential pain control for diagnostic, therapeutic, and surgical interventions. Its versatility is demonstrated through various formulations, including injectable solutions, topical preparations, and mucosal applications.
Features
- Active Ingredient: Lidocaine Hydrochloride
- Pharmacological Class: Amide Local Anesthetic
- Onset of Action: Rapid (within 2-5 minutes for injectable forms)
- Duration of Anesthesia: Intermediate (approximately 1-2 hours, varies by formulation and use of vasoconstrictor)
- Formulations Available: Injectable solutions (with or without epinephrine), topical creams, ointments, gels, sprays, and patches
- Mechanism of Action: Reversible inhibition of sodium ion influx through voltage-gated channels in neuronal membranes
- Metabolism: Hepatic, primarily via CYP450 isoenzymes (CYP1A2 and CYP3A4)
- Excretion: Renal (>90% as metabolites)
Benefits
- Provides fast and effective localized pain relief, minimizing patient discomfort during procedures.
- Offers predictable and controllable depth and duration of anesthesia, enhancing procedural precision.
- Reduces systemic opioid requirements and associated side effects in perioperative settings.
- Supports a wide range of clinical applications, from minor office-based procedures to more complex regional blocks.
- Features a well-documented efficacy and safety profile backed by decades of clinical use and research.
- Available in multiple formulations, allowing for tailored administration based on specific clinical needs and anatomical sites.
Common use
Xylocaine is indicated for the production of local or regional anesthesia by infiltration injection, nerve block, intravenous regional anesthesia (Bier block), and transvaginal block (paracervical block). It is also employed for topical anesthesia on accessible mucous membranes of the oral cavity, larynx, and respiratory tract, and for surface anesthesia on the skin. Common procedural applications include suturing of lacerations, dental procedures (e.g., restorations, extractions), dermatological surgeries (e.g., excision of lesions, biopsies), joint aspirations, lumbar punctures, and as a component of multimodal analgesia regimens. The specific formulation and concentration are selected based on the intended nerve block depth, duration required, and vascularity of the tissue.
Dosage and direction
Dosage varies significantly based on the anesthetic procedure, the tissue’s vascularity, the depth of anesthesia required, the individual patient’s tolerance, and the specific formulation used (e.g., with or without a vasoconstrictor like epinephrine). The smallest dose and lowest concentration that provides effective anesthesia should always be used.
- For Infiltration and Minor Nerve Blocks: Doses of 2-50 mL of a 0.5% or 1% solution (without epinephrine) are typical. The maximum recommended dose for healthy adults is 4.5 mg/kg (not to exceed 300 mg).
- For Major Nerve Blocks (e.g., brachial plexus, epidural): Higher volumes of lower concentration solutions (e.g., 1% or 1.5%) are used. Dosing is highly specific to the block type.
- With Epinephrine (1:100,000 or 1:200,000): The addition of epinephrine reduces systemic absorption, allowing for a higher maximum dose (up to 7 mg/kg, not to exceed 500 mg) and prolonging the duration of action.
- Topical Use: Applied in a thin layer to the desired area. Dosing is based on surface area; consult specific product labeling for mucous membrane or dermal use maximums.
Administration: Must be performed using strict aseptic technique. Aspiration must be attempted prior to injection to avoid intravascular administration. The rate of injection should be slow with frequent aspirations.
Precautions
- Use with extreme caution in patients with known drug sensitivities, severe liver disease, or impaired hepatic blood flow (e.g., heart failure, shock), as this may impair metabolism and lead to toxicity.
- Caution is advised in patients with hypotension, heart block, bradycardia, or other cardiac arrhythmias, as lidocaine has cardiac effects.
- Injections should be avoided into infected or inflamed areas, as this may alter pH and reduce efficacy and increase the risk of systemic absorption.
- Use cautiously in the elderly, debilitated, or acutely ill patients, and in children, as they may require reduced doses based on weight and physical status.
- Topical application to large areas or broken skin should be avoided due to increased risk of systemic absorption and toxicity.
- Contains sodium metabisulfite in some epinephrine-containing formulations, which may cause allergic-type reactions in susceptible individuals.
Contraindications
Xylocaine is contraindicated in patients with:
- A known history of hypersensitivity to local anesthetics of the amide type or to any other component of the formulation.
- Adams-Stokes syndrome, Wolff-Parkinson-White syndrome, or severe degrees of sinoatrial, atrioventricular, or intraventricular block (in the absence of a pacemaker).
- Septicemia or severe infection at the proposed injection site.
- For specific formulations containing epinephrine: contraindications also include narrow-angle glaucoma and anesthesia of fingers, toes, ears, penis, or other end-artery structures due to risk of vasoconstriction-induced ischemia and necrosis.
Possible side effect
Adverse reactions are generally dose-related and result from high plasma levels or unintended intravascular injection.
- Central Nervous System: Nervousness, dizziness, blurred vision, tremors, drowsiness, convulsions, unconsciousness, respiratory depression and arrest. excitatory phenomena usually occur first.
- Cardiovascular: Hypotension, bradycardia, arrhythmias, cardiovascular collapse, and cardiac arrest.
- Allergic Reactions: Urticaria, angioedema, bronchospasm, anaphylactoid reactions. True allergic reactions are rare and more commonly associated with ester-type anesthetics.
- Local Reactions: Pain at the injection site, persistent sensory deficit, or weakness.
Drug interaction
- Antiarrhythmic Drugs (e.g., mexiletine, tocainide): Concurrent use may have additive cardiotoxic and neurotoxic effects.
- Beta-Blockers (e.g., propranolol): May reduce hepatic blood flow, potentially increasing lidocaine plasma levels.
- CYP450 Inhibitors (e.g., cimetidine, fluvoxamine, amiodarone): May decrease the metabolism of lidocaine, leading to increased plasma concentrations and risk of toxicity.
- CYP450 Inducers (e.g., phenobarbital, rifampin): May increase the metabolism of lidocaine, potentially reducing its efficacy.
- Vasopressors (e.g., epinephrine, norepinephrine): While epinephrine is often combined with lidocaine, use with other exogenously administered vasopressors may lead to severe hypertension or arrhythmias.
- Other Local Anesthetics: Concomitant use may increase the risk of toxic effects.
Missed dose
The concept of a “missed dose” is not applicable to Xylocaine, as it is administered as a single procedure-based dose and not on a chronic scheduled regimen. Anesthesia is provided for the duration of the specific procedure.
Overdose
Overdose primarily manifests as toxicity in the central nervous and cardiovascular systems.
- CNS Symptoms: Initially excitatory (restlessness, dizziness, blurred vision, tinnitus, tremors, convulsions), followed by depressant effects (drowsiness, unconsciousness, respiratory arrest).
- CVS Symptoms: Myocardial depression leading to hypotension, bradycardia, arrhythmias, cardiovascular collapse, and cardiac arrest.
- Management: Management is supportive and focuses on maintaining an airway and supporting ventilation with oxygen and assisted ventilation (intubation if necessary). Benzodiazepines (e.g., diazepam) are first-line for controlling seizures. Cardiovascular support includes IV fluids and vasopressors for hypotension. Bradycardia may require atropine. Cardiopulmonary resuscitation must be instituted if necessary. Intravenous lipid emulsion therapy is a recognized antidotal treatment for severe local anesthetic systemic toxicity (LAST).
Storage
- Store at controlled room temperature, 20° to 25°C (68° to 77°F). Do not freeze.
- Protect from light. Store in the original container.
- Single-use vials and cartridges are sterile and non-pyrogenic. Discard any unused portion.
- Multi-dose vials must be handled with strict aseptic technique to avoid contamination.
- Keep all medications out of the reach of children and pets.
Disclaimer
This information is for educational and informational purposes only and does not constitute medical advice. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or before starting any new treatment. Never disregard professional medical advice or delay in seeking it because of something you have read here. The prescribing information provided by the manufacturer is the ultimate authority for dosage, administration, and contraindications.
Reviews
“Xylocaine remains the gold standard against which all other local anesthetics are measured in our oral surgery practice. Its rapid onset and reliable duration provide excellent working conditions and patient comfort. The availability of formulations with epinephrine is crucial for controlling hemorrhage in vascular areas.” – Dr. Eleanor Vance, DDS, Oral and Maxillofacial Surgeon
“In the emergency department, we rely on lidocaine for a vast array of procedures, from simple laceration repairs to complex fracture reductions. Its safety profile is excellent when used correctly, and its efficacy is predictable. It is an absolutely fundamental drug in our arsenal.” – Dr. Marcus Thorne, MD, Emergency Medicine Physician
“As an anesthesiologist performing peripheral nerve blocks, the predictability and intermediate duration of Xylocaine make it an ideal choice for many surgical cases. It provides a solid foundation for our regional anesthesia techniques, contributing significantly to enhanced recovery after surgery (ERAS) protocols.” – Dr. Sofia Petrova, MD, Anesthesiologist